Posts
Is direct neurofeedback a viable non-drug treatment option for ADHD?
/in Neurofeedback/by LindaAs the most common neurodevelopmental disorder, Attention-deficit hyperactivity disorder impacts an estimated 11% of children in school, with symptoms of inattention, hyperactivity, impulsivity and various cognitive dysfunctions often persisting into adolescence and adulthood. And thanks to modern neuroimaging technology, relatively distinct brain regions within the prefrontal cortex have been identified as having altered activity, accounting for the symptoms of ADHD. These disturbances in the networks of the brain have begun to come under further study when considering therapeutic interventions. Transcranial direct current stimulation (tDCS), aka direct neurofeedback, has shown promising effectiveness in both neuropsychological and neurodevelopmental disorders, especially ADHD.
Symptoms of inattention or being easily distracted is very common, as it is the mind’s natural tendency or default mode. It is actually wired for continuous distraction and a culture that values multi-tasking reinforces this wiring. Mindfulness, or the practice of narrowing our focus to a single-task or giving our undivided attention to the task at hand, is one way to train the mind to ‘pay attention’. However, this is sometimes easier said than actually done.
Now add trauma to this default mode of distraction. When the mind is overwhelmed by strong, and often uncomfortable emotions, the use of the natural, default distraction wiring of our brains can actually be of benefit as it provides relief from those emotions, albeit temporary, brief and fleeting. In fact, using conscious distraction techniques can actually keep us be safe from harm in the moment by moving us away from more unhealthy reactions to such powerful emotions, such as self-harming thoughts and behaviors including substance use.
The go-to approach to ADHD has been medication and behavioral modification therapy, yet the lack of long-term effects for both has been disappointing to those who suffer from the symptoms of this neurodevelopmental disorder. Such lack of long-term effects has generated renewed interest in neurofeedback in recent years as a promising method for improving neuropsychological and cognitive deficits in ADHD. Although more research may be required to determine the length of initial treatment along with the need for ongoing intermittent treatment to assess how long the benefits last, this non-invasive brain wave modulation intervention may just be a better approach while eliminating any medication side-effects!
If you would like to read more about the current state of the research on using direct neurofeedback for ADHD, click the link below:
Is expanding our capacity for compassion – for self and other – the key ingredient in healing through psychotherapy?
/in Talk Therapy/by LindaGrowing up in chaos challenges our equilibrium to seek control, wherever and whenever we can find it. This is a recipe for our perfectionist part to step forward and take control, driving us mercilessly to do more and better, striving for an ideal that does not exist. Ultimately, this is a recipe for failure, disappointment, anxiety, depression or worse. It wasn’t until I learned that as a spiritual being having a human experience that I am limited and flawed that acceptance began to flow in. This realization did not mean that I stopped striving to grow, do better and be a less judgmental human. It did mean that I had to reign in my perfectionist part and redefine my goals and ideals.
When acceptance began to flow for my limitations and mistakes, along with it came relief. I could stop setting myself up for failure and begin to release my grip on unrealistic expectations, not only for myself but of others. It opened the door to see and accept the limitations of others as a natural and universal aspect of being human. It also loosened the grip of the need to control, which calmed my overly developed responsible part, creating space for the capacity to simply be.
Part of my journey towards acceptance included work through psychotherapy that encouraged me to confront the chaos of my childhood and the traumatizing effects it had on all parts of me. I learned that perfectionism is a self-destructive and addictive belief system that fuels a primary thought that if I look perfect, and do everything perfectly, I can avoid or minimize the painful feelings of shame, judgment, and blame. Shame is the intensely painful feeling or experience of believing that we are flawed and therefore unworthy of love and belonging. Shame says ‘I am bad’ versus the feeling of guilt, which says ‘I did something bad’.
Having a compassionate witness, my psychotherapist, guide me along the sometimes slow and painful path back to wholeness, was mission critical for my healing. I came to learn that as children living through adverse experiences we adapt by turning against ourselves, which distorts our sense of self. We develop self-hatred as an adaptive response to protect our parents, which plants the seed that will grow the perfectionist part and set us on the path to work to improve our ‘bad’ self.
As I write this, my intention is not to blame, pass judgment on or shame parents. I am in a space of understanding and acceptance that humans do the best they can with what they know in the moment. However, the child goes through an unconscious development process that suggests: which is safer, for the child to believe that their parents are bad and they don’t love you or that they are incompetent and the world is not safe OR for the child to believe that there is something wrong with them, that they are not good enough or have something to be ashamed of? When we can understand that the fear of the loss of the attachment to our parents creates unendurable pain, then we can understand it is safer to turn on ourselves, because it leaves room for hope. Hope that if we work hard enough, we can change that bad part of ourselves and become lovable. This process creates the belief that if I can be good enough, I’ll be loved and belong.
What current research is offering is an approach to undoing the damage of this natural adaptive developmental process that is effective and embraced by people who suffer from shame. It is compassion-focused therapy. What is being demonstrated is that compassion is an essential capacity for growth, both inside and out. It is why I integrate a self-compassion assessment and meditation into my healing offering through talk therapy and offer a recording (here) for download for ongoing support. Having and truly offering compassion in therapy honors the experience of universal human suffering and now research is creating the evidence needed for compassion focused therapy to be embraced by the psychotherapy community.
To read more about where the research on compassion focused therapy currently stands, click the button below:
5 Intention-setting Ideas to Move Through Depression
/in Newsletter/by LindaNational Depression Education & Awareness Month!
As we move into the 8th month of learning to live with the Covid-19 virus, many of us continue to struggle with symptoms of depression emanating from the physical distancing and the many other losses we have experienced, including amongst others the loss of loved ones, loss of employment, inability to be with loved ones when they are sick or in the hospital, inability to give and receive hugs, and the changes to regular pleasurable activities that might have included going to the movies or taking an in-person yoga class with our favorite teacher.
There are many positives that are occurring during this time too, yet it can be difficult to focus on them when caught in the throws of depression. As my husband has been known to say “Not every day can be a home run”, it’s when more days than not that we feel like we struck out that becomes concerning.
According to the National Institute for Mental Health, “Depression is one of the most common mental disorders in the U.S.” There is no one cause for depression, yet it often stems from family history, major life changes, trauma, and/or stress, biological or other environmental factors. It impacts all people, regardless of age, race, ethnicity or gender, although prevalence rates are highest amongst adults identifying as two or more races.
Depression is typically treated with a combination of psychotherapy, medication and brain stimulation therapies.
Below I provide intention-setting ideas that might prove helpful to you or your loved ones when moving through depression:
- Breathe. Try Breath of Joy each morning. Standing with your feet a little wider than your hips, arms by your side to start. Take a 3-part inhale, raising both arms out in front of you on the first part of the inhale, moving both arms out to the sides at heart level on the second part of the inhale, and raising both arms to the sky on the third part of the inhale (YES, like you are conducting an orchestra), and then, as you exhale open your mouth, make a loud sighing out noise, as you swing your arms down along the sides of the body, fold the body over towards the ground while bending your knees. Repeat these steps while taking 3-5 more breaths. Afterwards, come back to standing with your arms along your sides, drawing your awareness to your hands, becoming aware of any sensations that might be present, while allowing your breath to return to a natural rhythm. Sense into how you can feel your energy moving!
- Set One Daily Goal. Make one goal that is especially meaningful to you. Start out small, knowing you can grow it if and when you are ready. Perhaps it is to make your favorite cup of tea in the morning and allow yourself 15 minutes (or more) to simply sit and enjoy drinking it. Or perhaps it is to use your mala or prayer beads to allow yourself to sit for 5-10 minutes saying your prayers first thing in the morning or the last thing before bed. Or it might be to read your favorite book or read the book that you have been meaning to read, but haven’t gotten to. And, the most important part is to give yourself a pat on the back when you accomplish your goad and NOT beat yourself up when you don’t. Be kind to yourself and simply set the goal again for the next day. Maybe the goal changes to simply be kind to myself!
- Be active. Exercise not only moves our body but also moves our e-motions (energy in motion). So, although it may be difficult or even feel impossible on some days to get up and move, moving helps! Walking as little as 15 minutes a day can help shift our energy and release some of the weight of depression. Gentle yoga is perhaps another option to try and, thanks to the pandemic, you don’t even need to leave the house to attend a virtual class.
- Reach out. The symptoms of depression tend to encourage us to withdraw and stay isolated, thinking that we don’t want to burden others with what we are going through. However, being with others helps us feel better and is one of the best coping strategies for moving through depression. And we don’t always have to put on our “happy mask” either. When we allow ourselves to be vulnerable and share our experiences, often we discover we are not alone in our challenges and, through sharing, we validate not only our experiences but the experiences of others. Humans were designed to feel good when helping others, so allow others to help by listening to us when we are not having one of those “home run” kind of days.
- Gratitude journaling. Practicing gratitude has been shown to increase our sense of peace and happiness. Again, when trying to identify what you might be grateful for, think small. This is another practice that will begin to grow as you continue to practice it. Some of the most mundane, routine things might begin to look and feel differently when sprinkled with gratitude. My most favorite items to add to my journal are: running hot water, a bed to sleep in, a roof over my head, and my furbabies who love me no matter what! I’d love to hear back from you what some of your favorites might be!
As always, if you try any of these intention-setting ideas for holistic health, I would love to hear about the impact they might have had for you. Please send me an email at linda@sanctuary4compassion.com to share!
Might transcranial direct current stimulation (aka direct neurofeedback) be an additional tool to reduce symptoms of depression as a result of the impact of the pandemic?
/in Neurofeedback/by LindaIf there is one silver lining to this pandemic it is the blossoming realization and acceptance of the fact that people need people! It is shining a light on the cultural ideal of independence and reflecting the shadow side of such an ideal. Human beings were designed to be interdependent, using relationships within their tribes and communities to grow and thrive. If independence was truly the healthy ideal, why aren’t more people thriving during this pandemic?
Use this time to reflect on the lessons being brought forward to us. If we embrace the fact that we need each other – and that it makes us feel good to help each other – than perhaps we can learn to be at ease with asking for help and support when we need it, knowing it will deepen our connections with others and make others feel good about themselves. What brings hope during these unexpected – and let’s just own it – scary times is collaboration and comradery. Knowing we are not alone – in our experiences, thoughts, and emotions – and that if we just have the courage to reach out, we will find relief.
Action is actually an antidote to fear. So, although the mind says withdraw, let the body lean in and reach out a hand – to call a friend, to pet an animal, to throw and catch a ball with a child and best of all to give and receive a hug with a loved one. You might even try your hand at writing, perhaps a letter or poem, to someone you care about and are unable to see in person at this time. Letting them know you are thinking about them and care about them might forever change their world in that immediate moment.
All of these acts of connection soothe the mind’s sense of disconnection. As neuroscience is demonstrating, our brains are wired for connection and, when we begin to experience disconnection, symptoms like depression start to develop. And the current pandemic conditions are only exacerbating any pre-existing sense of disconnection. Therefore, we need more tools that support the brain’s innate ability to reorganize towards health, beyond medications that bring so many unwanted side-effects. We need tools that reduce the fear signals in the brain so that action becomes more of an option when depressive symptoms loom.
Well, such a tool exists and a recent systematic review and meta-analysis of the research reflects that this tool is effective in the treatment of depression. Prior to this review, the results were mixed. However, now enough randomized clinical trials have been conducted and the cumulative data reflect that direct neurofeedback has achieved superior response and remission rates, warranting further large-scale clinical trials!
This information is vital as we continue to move through this pandemic and beyond. The lasting effects of the physical distancing required for our immediate physical health are still unknown at this time, yet history informs us that the psychological wounds may be deep. Acknowledging that symptoms of depression may be arising, whether within our own experience or witnessing it in others, helps to anticipate support might be needed along the healing path. Knowing about the treatment options facilitates choice throughout the journey.
To read more about this research click on the link below:
5 Intention-setting Ideas to Destigmatize Mental Health Challenges
/in Newsletter/by LindaPsychotherapy Day – September 25th
It might appear as an act of self-promotion, yet my intention is to share research, wherever and whenever possible, so everyone might move forward making more informed decisions when it comes to their own health, mind, body and spirit!
Psychotherapy works, especially when there is a genuine connection and deep understanding of the root causes to health challenges. And that deep understanding grows from the knowledge that it is not what is wrong with you, but what happened to you!
As I share again in this month’s Blog (see below), the research is unequivocal when showing the link between what happened to us (mental health) and the leading causes of morbidity and mortality (physical health). So, if we truly want to have a healthier world, we need to start with a focus on the mind and, if we do, the body will follow. This focus on the mind – and what traumatizes it – is the only way to break the transgenerational transmission of what ails the world.
Below I provide intention-settings idea to start to destigmatize mental health challenges to help shift the collective healthcare mindset from treating the long-term physical effects of trauma to prevention by inviting in more nurturing, compassion, understanding, belonging and acceptance into our lives:
- TALK about Mental Health. Do you remember the last time a conflict was resolved by silence? Neither do I! The only way to truly bring about collaboration and community is to talk things out. The act of talking takes courage and strength as it also requires us to listen deeply and with curiosity. Our minds want to make sense of the world, even when experiences may not be logical – we are meaning making vibrational beings. And often what makes the vibrations uncomfortable are the emotions of relationships. Human beings are wired for connection to others, as the pandemic has so clearly laid bare for us to feel. It is only when we can hold our relational emotions alongside of the rational thoughts that meaning mine opens wide for us to look into for the gold. Sometimes this is impossible to do without the support of another, who can welcome and hold the emotions with us, making space for the light. So it is my hope that all of us can set an intention to talk openly about our mental health, without shame, to remind us that we are not alone in our struggles.
- WRITE/BLOG about Mental Health. For those that are active on social media, I encourage you to set an intention to write or blog (or even vlog) about a small piece of your story, remembering that it is what happened to you, so you may begin to shine the light on any shame that you might be carrying. I like to compare shame as Toxic Mold that grows and thrives (and slowly kills) in the dark. If the light can reach it, it dies. When writing/sharing our stories, we are opening a window to let the light shine in and let the shame out. Remember the shame is not yours and no longer needs to be carried!
- Volunteer for Mental Health. If you always felt a heart tug to volunteer, yet haven’t found the “just right” organization or cause, perhaps consider mental health. As a starting point, visit the National Alliance on Mental Illness or Mental Health America websites for more information. Support is needed in all walks of life and all stages of life.
- Donate for Mental Health. If you find that you don’t have the time to volunteer right now, perhaps you might consider a financial donation. You might even look into whether or not your company might match your donation, as many organizations have such programs. Any energy expended with intention creates ripples in the universe far beyond what the human eye can see or mind can know, so every little bit counts!
- Read/Share Research on Mental Health. And last but certainly not least (and my favorite!) is read the research! And, after reading it, share it!! Remember the old Faberge Organics Shampoo commercial with Heather Locklear where she shared her experience with two friends . . . who shared it with two friends . . . etc., perhaps we can replicate that today by sharing something vitally important to the health of the world. It is this intention that might have the greatest impact on cutting short the public mental health crisis we have been challenged by for so many years. The research is crystal clear – work with the mind first to prevent diseases such as heart disease, diabetes, hypertension and cancer.
As always, if you try any of these intention-setting ideas for holistic health, I would love to hear about the impact they might have had for you. Please send me an email at linda@sanctuary4compassion.com to share!
Can meditation support your immune system, especially in light of the effects of COVID-19?
/in Yoga/by LindaAs someone that suffered with anxiety for most of my life, I am personally so grateful for my yoga practice, which includes various contemplative practices such as meditation. (Click here for a great image that reflects the many different types of contemplative practices.) What I found through the ongoing use of these tools is a consistent way to navigate stress to maintain my body, mind, and soul health. Stress is still present – and I no longer have any expectations of living a stress-free life – yet it no longer accumulates into an expression of anxiety.
Meditation is a very personal experience. It is the personal nature of the practice that can make it difficult to try and especially hard to maintain. There are also many different forms of meditation, so it definitely is not one-size-fits-all. Yet the intention behind meditation – to slow down the mind and help us detach from our thoughts – creates space. It is this space that can be scary. When we encounter stress, one of the most common tools humans go to in order to deal with the freeze/fight/flight response is distraction. We might distract ourselves by watching shows, eating, drinking, shopping, or one of the many other forms of impulsive behaviors that bring feelings of guilt and remorse along with them.
And yet more and more research is demonstrating the benefits of meditation, including how it can support our immune system functioning, which is vital right now in light of the pandemic. Meditation, whatever form of it that works best for you, helps to regulate the normal, natural human stress response, reducing the inevitable inflammation effects of that response. If we can find a form of meditation that we enjoy, then this tool can become the sharpest one in our toolkit and the one we consistently turn to when we feel anxiety building.
One of the more creative methods of meditations I utilize is journaling. This expressive writing tool has also been shown to reduce anxiety and depression. Relax Like A Boss, a website dedicated to wellbeing and stress, put together an ultimate guide to meditation journals. If you might consider this form of meditation, you can link to the guide here for tips on how to get started.
Contemplative practices do not have to be done for long periods of time, unless that works for you. Another one of my favorites is conscious deep breathing, and I do this several times a day for just a few minutes. It acts like a reset button for my nervous system. You might count how long you inhale and how long you exhale or you can include visualizations, such as colored light. You might add affirmations, such as inhaling peace and exhaling stress, if that helps give the thoughts in the mind the necessary mini vacation. Simply keep in mind that you cannot do it wrong!
I think what is most exciting is how research is looking at the body-mind connection more and more and not approaching the body and mind separately when working towards health. One recent review of the research literature focused on the interconnected physiological processes in the body that supports the continued inclusion – and expansion – of meditation in the treatment of diverse medical conditions. What they looked at more closely is the impact of stress on the gut microbiota and how meditation supports the health of our gut, leading to a healthier mind through the regulation of neurotransmitters. The research team recommended the integration of meditation into conventional health care and wellness models. If you would like to read more about this review, click the button below:
Can direct neurofeedback help individuals with a diagnosis of schizophrenia?
/in Neurofeedback/by LindaThe effects of the unprecedented coronavirus will be felt by all for a currently unknown period of time. The fear-driven behavioral responses that this pandemic has been producing is a reflection of how deep and strong our survival response goes. And, yet, at some point, relief will come in the form of a vaccine. However, there is another health challenge that stirs fear in the hearts of many, the life-long diagnosis of the severe mental disorder of schizophrenia.
One of my very first clients that I saw as a Marriage and Family Therapist Trainee carried a diagnosis of schizophrenia. My client challenged me to learn more about this disorder in order to provide the best quality of service I could at that point in my training. I learned that schizophrenia, although not as common as other mental disorders, affects feelings, thinking, and behaviors and the symptoms can be very disabling. Symptoms of schizophrenia are categorized using the medical terms of either positive, negative, or cognitive. Positive symptoms add and negative symptoms take away.
For example, positive symptoms might include hallucinations, delusions, or repetitive movements that are hard to control. Negative symptoms include reduced feelings of pleasure, reduced speech, apathy, reduced social drive and social interest, and loss of motivation. The underlying cause or causes of this severe mental disorder are still unknown and available treatments focus on eliminating the symptoms of the disease. The first line of attack as far as treatment is concerned is antipsychotic medications. Once a medication is found to work, then psychosocial treatments, such as therapy, is offered to help individuals learn and use coping skills. Research has shown that participating in such psychosocial treatments reduces relapses and/or hospitalizations; however, the most challenging aspect of treatment is nonadherence to medication. Therefore, a focus on increasing treatment adherence could have a positive effect on all impacted by this severe mental disorder.
Individuals with schizophrenia struggle to live life independently and improving this situation is a significant mental health priority. It seems as though the negative symptoms of this disorder are associated with poorer functional status and quality of life than are the positive symptoms and this may be because primary negative symptoms generally do not respond well to the antipsychotic medications currently available. Research has suggested that up to 60% of patients may have prominent clinically relevant negative symptoms that require treatment. With this information it then becomes more easily understandable why these individuals may not be compliant with their medications – because those medications don’t work for them. The question now is what is being done to support these individuals and address this unmet medical need?
Well, there is hope on the horizon. An article recently published in the Journal of the American Medical Association Psychiatry looked into the use of transcranial direct current stimulation (AKA direct neurofeedback) as an add-on therapy for negative symptoms of schizophrenia. In this double-blind randomized clinical trial of 100 individuals diagnosed with schizophrenia with predominant negative symptoms, results showed that this non-medication treatment was effective and safe in ameliorating negative symptoms.
If you would like to read more, click on the button below:
Compassion for Survivors of Trauma – a New View of Substance Use Disorder/Addiction!
/in Talk Therapy/by LindaI remember being assigned to read the book by Dr. Gabor Maté, In the Realm of Hungry Ghosts, while in graduate school and simply feeling gratitude, compassion and validation afterwards. I never believed in the medical model of addiction that describes the symptom of addiction as a chronic disease of the brain, even suggesting a genetic component to the disease, implying that if my parent(s) had addictions, most likely I would too. Now, don’t get me wrong, the brains of people who struggle with addiction are different, yet those changes are created as a response to the adverse childhood experiences (AKA TRAUMA) these people survived. And if your parents suffered from addictions when you were growing up, that experience is traumatic to a child!
I’ve written before about the impact of adverse childhood experiences, especially on physical health later in life as well as addiction; however, I felt compelled to revisit it again when I learned of research that found over 96% of the study participants suffering from substance use disorders, including prescription opioids, nicotine, and cocaine, had trauma histories. When comparing the groups based upon their drug of choice, the prescription opiate group reported more traumatic childhood experiences than the other groups and a younger age of their first adverse childhood event. So, when you learn about the underlying dynamics associated with substance use, the thought of “Just Say No” to drugs seems crazy!
Trauma comes in many packages and I’m grateful that the new California Surgeon General (Dr. Nadine Burke Harris) is focusing on early childhood, health equity and Adverse Childhood Experiences and toxic stress as her key priorities. (For more information on the ACEs Aware initiative, visit www.ACEsAware.org.) It is time to stop blaming the victims and participate in bringing this information forward in order to educate. What we don’t know, we don’t know. However, once we know better, we can do better. With this knowledge, we can bring more empathy and compassion in our interactions with people that struggle with substances. We can take extra steps to explain this new research to them, validating their experiences and bringing them hope that they can heal from these past traumatic experiences and release their attachment to something that is harmful to them. We can empower them to explore various healing modalities, such as psychotherapy, neurofeedback, meditation, hypnosis, guided imagery, and expressive arts, such as yoga, writing and drawing, all of which have been shown to support post-traumatic growth.
To read more about this research, click on the box below:
Might direct neurofeedback reduce impulsive behaviors?
/in Neurofeedback/by LindaThe symptom of impulsivity can be found listed under several mental/behavioral health diagnoses, including but not limited to intermittent explosive disorder, substance abuse, OCD, PTSD and binge eating disorder. When the Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5™) was published in 2013 and included binge eating disorder, I finally felt validated and, at the same time, gratitude for discovering yoga, which helped to reduce my anxiety and my out-of-control eating, especially in light of the fact that I didn’t want to start taking any prescription medications.
My relationship with food has been a long and winding road. I have memories when I was 4 or 5 of sitting at my kitchen table by myself, long after everyone else finished eating and was allowed to move on, because I was not allowed to leave the table until I finished everything on my plate, including those horrible green vegetables. I tried every trick in the book, including slipping some to the dog under the table and putting some in my mouth, wiping my mouth with a napkin and spitting what was in my mouth into the napkin. I also hear my parents in my mind saying “Eat your food! There are people starving in Africa” and thinking to myself “Great, send them my food!”.
From there, after my parents got divorced, food became scarce for most of my adolescence. My parents’ divorce and subsequent relationship was very contentious, pushing me into the land of anxiety. I began to worry about where my next meal would be coming from and if it would be enough. The pattern that grew from there involved eating large amounts of food (even if I wasn’t hungry) when food was available and eating very quickly (to ensure I got enough before it disappeared). I also have memories as a young adult where I would eat my meal very quickly and then eat what was left by others on their plates.
As time passed, my relationship with food changed when my weight began to increase. At this point, I would not allow myself to eat anything until the end of the day, after I had taken care of everyone else’s needs on my list. Only then, almost like a reward for completing my “To Do” list for others and my sense of self-restraint or control, would I allow myself the indulgence of fulfilling one of the most basic human needs. What didn’t change at this point though, was the speed in which I ate and the amount of food I would eat!
I then ventured into the many ‘diets’ being promoted. My weight began to yo-yo. My life felt so out-of-control as did I! It wasn’t until I discovered yoga that I found myself in a space to really confront this unhealthy relationship I had with food, facing the fears lying beneath my journey in the land of anxiety. And even with the support of my yoga practice (and a boost from some hypnotherapy), it took me many more years to see food as simply a source of energy for my body, like gas or electric for a car.
So how excited was I when I read the recent promising research on using direct neurofeedback (i.e., transcranial direct current stimulation or tDCS) to reduce impulsive behaviors! Although it is not exactly clear how it does so, a positive effect was found in 74 out of 92 research studies. It warms my heart to learn that there is an alternative to prescription medications, something that specifically supports the brain’s innate ability to reorganize itself towards health, and does so relatively quickly.
If you would like to read a little more on this research, click on the box below:

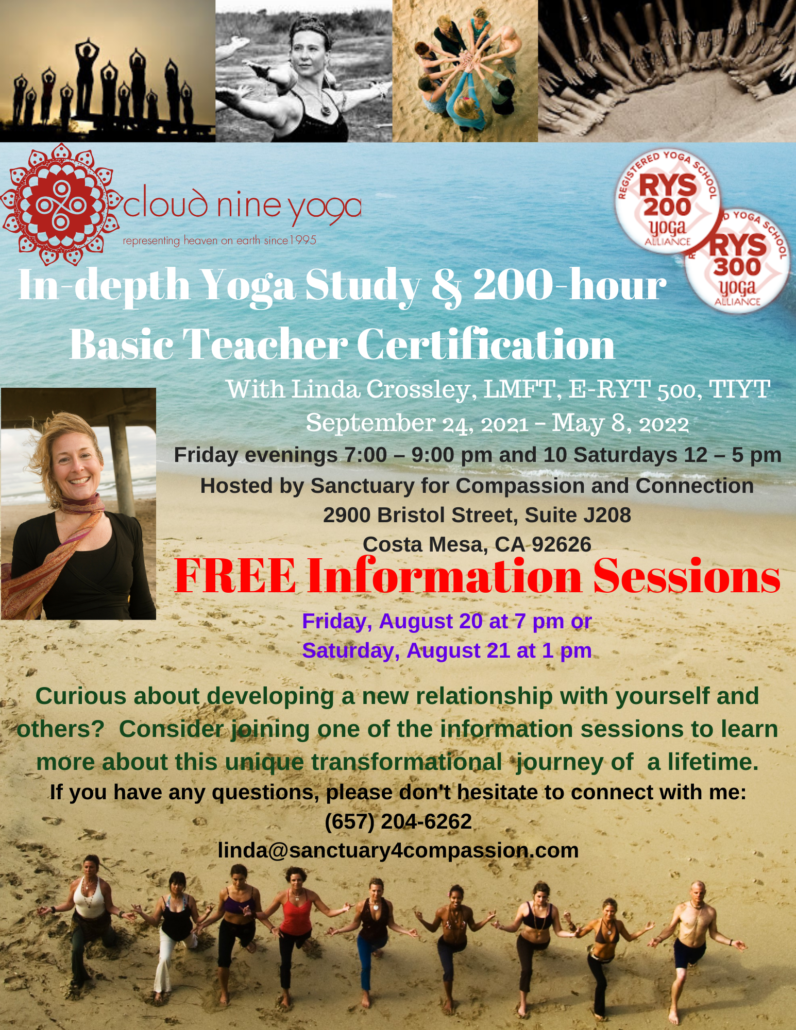
Office located at:
2900 Bristol Street, Suite J208
Costa Mesa, CA 92626
Hours:
Monday-Wednesday
9:00 am – 9:00 pm
Thursday-Friday
12:00 pm – 5:00 pm
Saturday
9:00 am – 12:00 pm
Connect with me:
LINDA CROSSLEY, MBA,
LMFT*, E-RYT 500®
*License # LMFT93390
Serving Orange County, CA
To leave a confidential voice mail,
please call (714) 707-1277
For all other inquiries, please call
(657) 204-6262